By Laura Cassiday
June 2015
- Nutritionists have long vilified saturated fat for its propensity to raise LDL (“bad”) cholesterol levels in the blood.
- Although initial epidemiological studies associated saturated fat intake with heart disease risk, subsequent studies have failed to confirm the link.
- Saturated fat raises HDL (“good”) cholesterol levels, perhaps ameliorating its effects on LDL cholesterol.
- An unintended consequence of a low-fat diet may be increased carbohydrate intake, which could actually raise heart disease risk compared with a higher-fat diet.
In the early hours of September 24, 1955, US President Dwight D. Eisenhower suffered a massive heart attack. The popular president and war hero was visiting in-laws in Denver, Colorado, where he had enjoyed 27 holes of golf before retiring early that evening with what he thought was indigestion. Although Eisenhower recovered and went on to win a second term in office, his sudden incapacitation heightened public awareness of the growing epidemic of cardiovascular disease. Once a rare ailment, by the 1950s heart disease had become the leading cause of death in the United States. What diet, lifestyle, or other factors were responsible for this dramatic change? People were looking for a scapegoat, and nutritional scientists were soon to provide one.
Researchers were already beginning to implicate dietary fats, particularly saturated fats, in cardiovascular disease. The logic went like this: Saturated fats such as those found in butter, meat, cheese, and eggs raised serum cholesterol in laboratory animals and humans. Because cholesterol is a major component of atherosclerotic plaques, and early studies had linked high serum cholesterol levels to heart disease, then saturated fat must cause heart disease.
In 1970, well-known nutrition researcher Ancel Keys, who developed the US Army K-rations during World War II, published his famous Seven Countries Study (Keys, A., ed., Circulation 41(4 Suppl.):I 1–200, 1970). Keys compared the health and diet of 12,700 middle-aged men in Italy, Greece, Yugoslavia, Finland, the Netherlands, Japan, and the United States. His conclusion: Populations that ate large amounts of saturated fats in meat and dairy had more deaths from heart disease than those that ate mostly grains, fish, nuts, and vegetables.
When the US Department of Agriculture (USDA) and the US Department of Health and Human Services jointly released the first Dietary Guidelines for Americans in 1980, saturated fat played a leading villainous role. The Guidelines, which are updated every five years by an expert committee and form the basis of US nutritional policy, advised citizens to “avoid too much fat, saturated fat, and cholesterol.” The United Kingdom issued similar dietary guidelines in 1984. Both guidelines recommended reducing overall fat consumption to 30% of total calories, and saturated fat to no more than 10% of calories—values that have remained essentially unchanged in subsequent iterations.
Yet recent evidence, as well as reevaluation of older studies, has questioned whether dietary fat is really as bad as the experts have been saying for the past three decades. A paper published in the January 29, 2015, edition of the BMJ’s Open Heart examined the data on fat and cardiovascular disease available to US and UK regulatory committees at the time the 1980 and 1984 guidelines were issued (Harcombe, Z., et al., https://dx.doi.org/10.1136/openhrt-2014-000196, 2015). The analysis revealed that the six randomized controlled trials available back then did not provide sufficient evidence that cutting total fat or saturated fat intake reduces deaths from heart disease. The authors conclude that the “dietary advice not merely needs review; it should not have been introduced.”
Now, 35 years since the first guidelines were issued, a continued lack of consistent evidence showing that dietary saturated fats cause heart disease, as well as an improved understanding of how fats affect different types of cholesterol particles in the body, has cast doubt on the government’s recommendations. Some experts say it is time to increase or even nix the limit on saturated fat found in the Dietary Guidelines for Americans. Doing so would have far-reaching consequences, from changing school lunch programs to readjusting the priorities of food manufacturers. Although the Scientific Report of the 2015 Dietary Guidelines Advisory Committee recommends maintaining the status quo with regard to saturated fat, the official guidelines will not be released until the third quarter of 2015. Meanwhile, some experts argue that the current recommendations on saturated fat are not only ineffective at reducing rates of cardiovascular disease, obesity, and type 2 diabetes, they may actually be doing more harm than good.
Changing diets
Before 1910, people in the United States used butter and animal fats almost exclusively for cooking and baking. These were rich in saturated fatty acids, which are defined chemically as fat molecules with no double bonds between carbon atoms of the hydrocarbon chain. Saturated fats are solids at room temperature. In contrast, most vegetable oils such as corn, soybean, and canola/rapeseed oils are liquids at room temperature and contain primarily unsaturated fats, either monounsaturated (one double bond in the hydrocarbon chain) or polyunsaturated (multiple double bonds). In 1910, cooking with vegetable oils was virtually unheard of—oils were instead used to make soaps, candles, lubricants, and other nonedible products.
But then a dramatic change occurred. As the process of hulling and pressing seeds and beans was mechanized, vegetable oils became cheaper than raising and slaughtering animals for butter or animal fat. Aggressive marketing by vegetable oil companies claimed that vegetable oils were a more healthful, easier-to-digest, and more sanitary alternative to animal fats. In 1911, Proctor & Gamble applied for a US patent for the process of hydrogenating vegetable oil; in other words, adding hydrogen molecules to remove some of the double bonds in unsaturated fatty acids. This process enabled the production of solid vegetable oils such as Crisco shortening and margarine, increasing the shelf lives of oils and paving the way for their use in baking and frying.
From 1909–1999, consumption of soybean oil in the United States increased by more than 1,000-fold per person and margarine consumption increased 12-fold, whereas consumption of butter and lard decreased by about four-fold each (Blasbalg, T. L., et al., https://dx.doi.org/10.3945/ajcn.110.006643, 2011). These changes in consumption are depicted in Fig. 1.
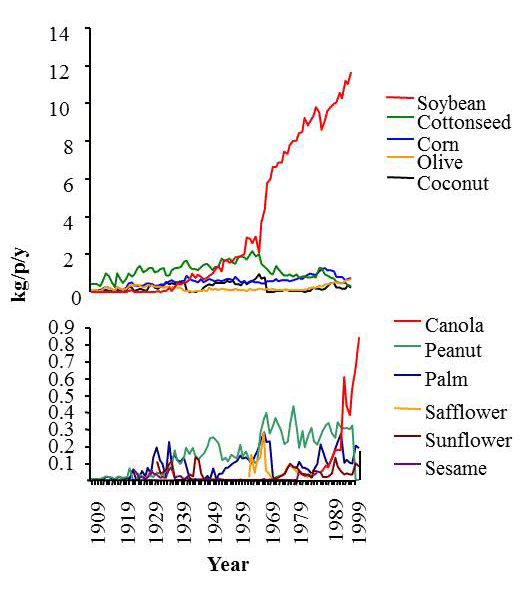
FIG. 1 Trends in the apparent consumption of a. major fat categories between 1909-C and 1999, unadjusted for changes in total energy consumption; b. vegetable and seed oils between 1909-C and 1999, unadjusted for changes in total energy consumption. Reprinted with permission from Blasbalg, T. L., et al., “Changes in consumption of omega-3 and omega-6 fatty acids in the United States during the 20th century.” Am. J. Clin. Nutr. 93:950–962, 2011. DOI: 10.3945/ajcn.110.006643. © US Government.
Yet at the same time these supposedly “heart-healthy” changes were taking place, heart disease was on the rise. In the past decade, deaths from heart disease in the United States have dropped (Mozaffarian, D., et al., https://dx.doi.org/10.1161/CIR.0000000000000157, 2015), mainly due to reduced smoking and improved emergency care, but heart disease remains the No. 1 killer of people worldwide (World Health Organization, Fact Sheet No. 317, 2015).
Another major dietary change that has taken place in the past 50 years is the substitution of fats in the diet with carbohydrates such as pasta, grains, sugar, fruit, and starchy vegetables. According to Nina Teicholz, author of The New York Times bestselling book The Big Fat Surprise: Why Butter, Meat & Cheese Belong in a Healthy Diet, in 1960 approximately equal numbers of calories in the American diet came from fats and carbohydrates (40% each). Then, the low-fat diet craze hit the nation. People began avoiding foods such as full-fat dairy, eggs, and red meat and substituted low-fat or fat-free foods, many of which had added sugar to make them more palatable. Now, carbohydrates comprise about 50% of total calories in the US diet, while total fats are down to about 30%. Meanwhile, saturated fat consumption has dropped to about 11% of total calories (Wright, J.D., and Wang, C.-Y., NCHS Data Brief, No. 49, 2010).
Ironically, these values are right in line with the US government’s recommendations, yet obesity, heart disease, and diabetes continue to be problems. “The experts like to claim that Americans are fat and unhealthy because they don’t follow the guidelines—it’s their own fault,” says Teicholz. “But if you look at the broad data it’s very clear that, in terms of macronutrients, we have been following the guidelines.”
Fat facts
The reason dietary fats garnered such a bad reputation in the 1950s is that a high fat intake, particularly saturated fat, raises the level of total cholesterol in the blood, which is a risk factor for heart disease. But it wasn’t until the 1980s that researchers began to appreciate that all forms of cholesterol are not created equal.
Cholesterol and other fats are transported in the bloodstream by different lipoprotein complexes. Low-density lipoproteins (LDL), or “bad cholesterol,” can contribute to plaques in the arteries, increasing the risk for cardiovascular disease. However, high-density lipoproteins (HDL), or “good cholesterol,” have the opposite effect: They transport cholesterol away from artery walls, reducing the risk of heart disease.
The propensity of saturated fat in the diet to raise LDL cholesterol is what nutrition researchers have found so worrisome. In contrast, mono- and polyunsaturated fats tend to lower LDL cholesterol, which is why the Dietary Guidelines recommend replacing saturated fats in the diet with unsaturated fats. However, saturated fats also raise HDL cholesterol more than any other type of fat, possibly mitigating the harmful effects of LDL cholesterol. Trans fats, the intended replacement for saturated fats, raise LDL cholesterol even more than saturated fats, while lowering HDL cholesterol levels.
Total cholesterol levels in the blood do not always correlate well with a person’s risk for heart disease risk because the measurement includes both LDL and HDL cholesterol. A more sensitive and specific predictor is the ratio of total cholesterol to HDL cholesterol (total:HDL) (Kinosian, B., et al., J. Investig. Med. 43:443–450, 1995). Mono- and polyunsaturated fats lower total:HDL cholesterol, suggesting that they reduce the risk of heart disease. In contrast, trans fats increase the ratio, presumably increasing the risk of heart disease. However, because of their effects on both types of cholesterol particles, saturated fats neither raise nor lower total:HDL cholesterol (Mensink, R. P., et al., Am. J. Clin. Nutr. 77:1146–1155, 2003), suggesting little or no effect on cardiovascular disease risk.
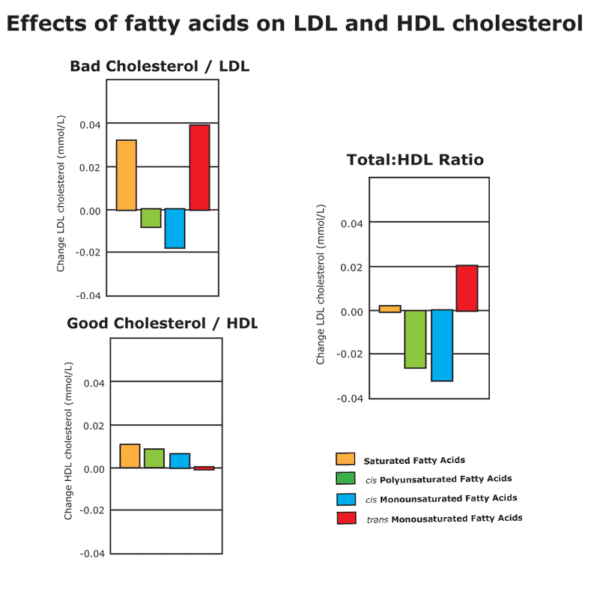
FIG. 2 Effects of fatty acids on LDL and HDL cholesterol. (Left) Saturated and trans fats increase the serum levels of LDL, or “bad,” cholesterol. (Center) Saturated and unsaturated fatty acids increase HDL, or “good,” cholesterol. (Right) Unsaturated fats decrease the ratio of total cholesterol to HDL, indicating a reduction in heart disease risk. Trans fats increase this ratio, while saturated fats do not substantially increase or decrease the ratio. Credit: Gerald McNeill, prepared from data in Mensink, R. P., et al. , “Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials.” Am. J. Clin. Nutr. 77: 1146-1155, 2003.
In the 1990s, Ronald Krauss, director of atherosclerosis research at Children’s Hospital Oakland Research Institute in Oakland, California, USA, and a practicing physician, discovered that the situation is even more complex than “good” and “bad” cholesterol. Krauss developed a technique to separate LDL cholesterol into different types of particles: large, buoyant particles and small, dense particles. As it turns out, the small, dense LDL particles are more strongly associated with cardiovascular disease risk than the large, buoyant particles (reviewed in Berneis, K. K., and Krauss, R. M., https://dx.doi.org/10.1194/jlr.R200004-JLR200, 2002). The small LDL particles are more easily oxidized and more likely to trigger inflammation and plaque formation, leading to atherosclerosis.
Krauss has studied the effects of diet on these two LDL subpopulations. “What we found is that the small, dense form of LDL is raised by carbohydrates, and the larger form is raised by saturated fat,” he says. “And so we started to wonder if the dietary effects of saturated fat on LDL cholesterol could be misleading in terms of heart disease risk.” Krauss notes that because the larger particles contain more cholesterol, they contribute more to the measurement of LDL cholesterol in the blood than the smaller particles. Therefore, total LDL cholesterol measurements, commonly used by doctors to gauge heart disease risk, could fail to identify the patients at highest risk.
Although methods for measuring specific types of LDL are now commercially available, the tests aren’t widely utilized, says Krauss. “The testing is inexpensive, but it’s not well known, and there’s a lot of controversy regarding its clinical use,” says Krauss. “But for people who are concerned about their heart disease risk, have other risk factors, or are considering treatments, it provides a much finer tool than the blunt LDL cholesterol measurement, which can really miss the boat in terms of LDL particle subtypes.”
Not everyone is convinced that particle size matters, however. “I don’t think we can say that any LDL is good,” says Penny Kris-Etherton, distinguished professor of nutrition at The Pennsylvania State University. “Some people are saying the large particles are lessharmful, but the American College of Cardiology and the American Heart Association are saying just look at total LDL. All of it’s bad, and you want to get it down.” Kris-Etherton notes that the American Heart Association’s dietary recommendations for lowering cholesterol include reducing saturated fat to only 5–6% of total calories, even lower than the 10% recommended by the USDA.
The problem with epidemiology
When the first Dietary Guidelines for Americans were released in 1980, few clinical trials had been conducted on saturated fat and heart disease risk, and those that had been conducted were inconclusive. As a result, the first Dietary Guidelines Advisory Committee relied almost exclusively on epidemiological data to formulate their recommendations for saturated fat.
In this arena, Keys’ Seven Countries Study loomed large. After all, Keys had shown that people from countries that consumed higher amounts of saturated fats (for example, the United States and Finland) died from heart disease at a greater rate than those who ate less saturated fat (such as Japan and Greece). However, epidemiological studies can only prove correlation, not causation. It’s possible that other diet or lifestyle factors could explain the difference in heart disease deaths. For example, a reanalysis of the Seven Countries Study conducted in 1999 concluded that sugar consumption correlated more strongly than saturated fat intake with heart disease deaths (Menotti, A., et al., Eur. J. Epidemiol. 15:507–515, 1999). Populations that ate lower amounts of saturated fat also tended to consume fewer sugary desserts and pastries.
In recent years, the Seven Countries study has been criticized and largely discredited because of troubling methodological problems. Keys apparently included only those countries that would confirm his hypothesis that saturated fat causes heart disease, while excluding countries such as France and Switzerland that consume relatively large amounts of saturated fat yet do not suffer high rates of heart disease deaths. Also, although 12,770 men were asked about their diet and followed for 10 years to see if they died of heart disease, the researchers actually sampled the diets of only about 500 of them. One of the diet surveys in Greece occurred during Lent, when many people were deliberately avoiding animal products. And, finally, although a diet low in saturated fat correlated with fewer deaths from heart disease, saturated fat intake had no effect on total deaths. In other words, people from countries that consumed low amounts of saturated fat had just as high a risk of dying, but they died from other causes.
Other epidemiological studies, as well as controlled clinical trials, have produced conflicting results as to whether saturated fat intake modulates heart disease risk. Pooling data from multiple studies (called a meta-analysis) can help researchers identify patterns when individual studies disagree. In 2010, Krauss and his colleagues performed a meta-analysis of 21 prospective cohort studies of generally healthy people who differed in saturated fat intake (Siri-Tarino, P. W., et al., https://dx.doi.org/10.3945/ajcn.2009.27725). The meta-analysis revealed that among the almost 350,000 people included in the 21 studies, a higher intake of saturated fat was not associated with an increased risk of coronary heart disease, stroke, or cardiovascular disease.
More recently, researchers led by Rajiv Chowdhury at the University of Cambridge, in the UK, performed a meta-analysis of 32 observational studies that examined people’s intake of different types of fat and their risk of heart disease (https://dx.doi.org/10.7326/M13-1788, 2014). Because study participants sometimes misreport what they eat, the researchers also analyzed 17 studies that actually measured fatty acids circulating in people’s blood as an indication of their diet. In addition, the researchers examined 27 randomized controlled trials of supposedly beneficial fatty acid supplements (e.g., omega-3 polyunsaturated fatty acids) given to prevent heart attacks. In total, the meta-analysis included more than 600,000 participants from 18 countries.
Chowdhury and his colleagues found no significant associations between dietary, circulating, or supplementary fatty acids and heart disease risk, with the exception of dietary trans fats, which slightly increased risk in the five studies analyzed. “Current evidence does not clearly support guidelines that encourage high consumption of polyunsaturated fatty acids and low consumption of total saturated fats,” the authors conclude. “Nutritional guidelines on fatty acids and cardiovascular guidelines may require reappraisal to reflect the current evidence.” A revision of the paper retracted its initial conclusions on polyunsaturated acids because of an erroneous analysis of omega-3 polyunsaturated acids, which were indeed associated with cardiovascular benefit. However, the study’s conclusions regarding saturated fat remain unchanged.
Critics of the Krauss and Chowdhury reports point out that the meta-analyses lumped together studies that replaced saturated fat with polyunsaturated fat and those that replaced saturated fat with carbohydrates. “When you look at meta-analyses that actually distinguish between the replacement components, there’s a clear benefit of replacing saturated fat with polyunsatured fat but not of replacing saturated fat with carbohydrates,” says Alice Lichtenstein, professor of nutrition science and policy at Tufts University and vice-chair of the 2015 Dietary Guidelines Advisory Committee. In other words, saturated fat may be bad for you compared with polyunsaturated fat, but its negative effects could be masked by the fact that carbohydrates are even worse.
Krauss agrees that the overall dietary context is important to consider when interpreting these studies. When people are asked to lower their intake of one nutrient, such as saturated fat, they compensate by increasing their intake of another, such as carbohydrates. “In the context of our findings we tried to explain that saturated fat per se cannot easily be connected to adverse effects,” says Krauss. “We’re trying to broaden the discussion from this monomaniacal focus on one single chemical in foods, saturated fat.”
Time for a change?
With an updated version of the Dietary Guidelines for Americans set to be released in the third quarter of 2015, some researchers were hopeful that, given new evidence over the past five years, saturated fat would be at least partially exonerated. However, the Scientific Report of the 2015 Dietary Guidelines Advisory Committee continues to identify saturated fat as a “nutrient of concern for overconsumption” that should be limited to less than 10% of total calories. Although the federal government will have the final say on the Dietary Guidelines, it is unlikely that the guidelines will diverge significantly from the scientific report of the committee.
Krauss considers it a good sign that the Dietary Guidelines Advisory Committee hasn’t recommended cutting saturated fat even further, down to the Draconian 5–6% of total calories suggested by the American Heart Association. “Ten percent is a reasonable amount of saturated fat,” he says. “But rather than the notion that people should be fanatically adding up the saturated fats in their diet and figuring out how much they should be eating, people should be more concerned about their overall dietary pattern and the types of foods they choose.”
He notes that the type of food in which the saturated fat is contained, or the “food matrix,” may influence heart disease risk. For example, some studies suggest that fermented dairy products such as cheese—often avoided because of its high saturated fat content—may contain specific saturated fatty acids that, in the context of other components in the cheese, may actually lower the risk of heart disease and type 2 diabetes.
With regard to food choices, Krauss was dismayed when press coverage of his 2010 meta-analysis tended toward sensational headlines proclaiming it’s okay to load up on sticks of butter and triple burgers with cheese. “That’s not the message,” says Krauss. “The message is to make food choices that are balanced in the overall diet and not to consider any given food the salvation of health or the kiss of death.”
Teicholz believes that, in light of recent evidence, the Dietary Guidelines should ditch limits on saturated fat, but she thinks that change is unlikely to occur. “We’re in the third generation of scientists who believe fat, and especially saturated fat, is bad for health,” she says. “The bias is deeply entrenched, and it’s very hard to reverse that.”
She points out that the Scientific Report of the 2015 Dietary Guidelines Advisory Committee states that a healthy dietary pattern should be one low in lean meat (both for dietary and environmental reasons). “They’re recommending an essentially meatless diet for all Americans, and that’s based primarily on this saturated fat concept,” she says. Not only is a vegetarian diet impractical for many, but Teicholz worries that people will get the erroneous message that it’s more healthful to replace meats with carbohydrates such as rice, pasta, or bread. Counter to popular perception, carbohydrates contribute more to obesity and cardiovascular disease risk than saturated fat, she says.
Gerald McNeill, vice president of research and development at IOI Loders Croklaan, an edible oil supplier with US headquarters in Channahon, Illinois, notes that calls to further limit saturated fat would necessitate drastic changes in the US diet. “Seventy-five percent of all dietary saturated fat is contained in meats, dairy products, and eggs,” he says. “To reduce saturated fat to 5% of total calories, a reduction of approximately 65% of these foods in the diet is required.” McNeill notes that, in addition to the decimation of the meat and dairy industries, the near-elimination of these foods would deprive people of important sources of vitamins, minerals, proteins, and fats. “Implementation of such a recommendation could plunge the dietary status of the nation into the dark ages,” he predicts.
Teicholz questions the wisdom of replacing saturated fats with polyunsaturated fats, as recommended by the Dietary Guidelines. Although polyunsaturated fats do lower LDL cholesterol and total:HDL cholesterol, their double bonds make them more prone to oxidation than saturated fats, especially when heated during food preparation. Aldehydes produced from polyunsaturated fats can react with DNA, proteins, and lipids in the body, possibly interfering with their functions (Grootveld, M., et al., Inform 25:614–624, 2014). Some studies suggest that omega-6 polyunsaturated fatty acids, contained in many vegetable oils, increase inflammation and even promote diseases such as cancer, cardiovascular disease, and type 2 diabetes (reviewed in Lawrence, G. D., https://dx.doi.org/10.3945/an.113.003657, 2013). Teicholz calls the massive increase in vegetable oil consumption over the past century “the biggest change in the American diet”—a dietary experiment for which we may not yet appreciate the consequences.
In a promising sign that the Dietary Guidelines Advisory Committee is, in some instances, willing to change its course, the 2015 Committee recommended withdrawing its longstanding warnings about dietary cholesterol. This reversal comes after years of studies showing that eating foods rich in cholesterol, like eggs, doesn’t actually raise cholesterol levels in the blood or contribute to heart disease. Perhaps in 2020 saturated fat will join cholesterol in exoneration, but the pervasive messages that these dietary components are bad for health will likely take decades to erase in the minds of nutritionists and the general public alike.
Laura Cassiday is a science writer for Inform magazine. She is based in the Denver area and can be reached at laura.cassiday@aocs.org.
Information
Berneis, K. K., and Krauss, R. M. (2002) “Metabolic origins and clinical significance of LDL heterogeneity.” J. Lipid Res., 43:1363–1379. https://dx.doilorg:10.1194/jlr.R200004-JLR200.
Blasbalg, T. L., et al. (2011) “Changes in consumption of omega-3 and omega-6 fatty acids in the United States during the 20th century.” Am. J. Clin. Nutr. 93:950–962. DOI: 10.3945/ajcn.110.006643.
Chowdhury, R., et al. (2014) “Association of Dietary, Circulating, and Supplement Fatty Acids with Coronary Risk.” Ann. Intern. Med. 160:398–406. DOI: 10.7326/M13-1788.
Harcombe, Z., et al. (2015) “Evidence from randomised controlled trials did not support the introduction of dietary fat guidelines in 1977 and 1983: a systematic review and meta-analysis.” Open Heart 2:e000196. DOI: 10.1136/openhrt-2014-000196.
Grootveld, M., et al. (2014) “Detection, monitoring, and deleterious health effects of lipid oxidation products generated in culinary oils during thermal stressing episodes.” Inform 25:614–624.
Keys, Ancel, ed. (1970) “Coronary Heart Disease in Seven Countries.” Circulation 41(4 Suppl.):I 1–200.
Kinosian, B., et al. (1995) “Cholesterol and coronary heart disease: predicting risks in men by changes in levels and ratios.” J. Investig. Med. 43:443–450.
Menotti, A., et al. (1999) “Food intake patterns and 25-year mortality from coronary heart disease: cross-cultural correlations in the Seven Countries Study.” Eur. J. Epidemiol. 15:507–515.
Mensink, R. P., et al. (2003) “Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials.” Am. J. Clin. Nutr. 77:1146–1155.
Mozaffarian, D., et al. (2015) “Heart Disease and Stroke Statistics—2015 Update. A Report from the American Heart Association.” Circulation 131:434–441. DOI: 10.1161/CIR.0000000000000157
Scientific Report of the 2015 Dietary Guidelines Advisory Committee. Downloaded from www.health.gov/dietaryguidelines/2015-scientific-report.
Siri-Tarino, P. W., et al. (2010) “Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease.” Am. J. Clin. Nutr. 91:535–546. DOI: 10.3945/ajcn.2009.27725, 2010.
Teicholz, Nina. The Big Fat Surprise: Why Butter, Meat & Cheese Belong in a Healthy Diet. New York: Simon & Schuster, Inc., 2014.
World Health Organization, Fact Sheet No. 317, “Cardiovascular Disease,” Updated January 2015. Downloaded from www.who.int/mediacentre/factsheets/fs317/en.
Wright, J.D., and Wang, C.-Y. (2010) “Trends in intake of energy and macronutrients in adults from 1999–2000 through 2007–2008.” NCHS Data Brief, No. 49. Downloaded from www.cdc.gov/nchs/data/databriefs/db49.pdf.
Sidebar
Saturated and trans fat alternatives
The fact that dietary guidelines in many countries continue to vilify saturated fats, along with more recent warnings about trans fats, has put many food manufacturers between a rock and a hard place. “Partially hydrogenated vegetable oils were meant to replace saturated fats,” says Nina Teicholz, author of The New York Times bestselling book The Big Fat Surprise: Why Butter, Meat & Cheese Belong in a Healthy Diet. “Now, because of the trans fat scare, the food industry can’t use partially hydrogenated vegetable oils, which the FDA is on the verge of banning anyway, and they can’t use saturated fats because people are so afraid of them.”
Solid fats are particularly needed in the bakery industry. “In bakery products, fat plays several roles beyond just flavor and succulence,” says Charles Speirs, baking science and technology manager at Campden BRI, a membership-based food and beverage research facility with headquarters in Gloucestershire, UK. “For example, in cakes you need saturated fats to help sustain the bubble structure that you get during rising and baking.” Speirs says that liquid vegetable oils do not have the same functional properties and therefore cannot replace saturated fats in products such as cakes, cookies, and pastries.
In his research at Campden BRI, Speirs has explored the use of next-generation emulsions to reduce saturated fat in bakery products. Ordinary water-in-oil emulsions don’t have the same properties as hard fats such as butter or lard. So Speirs and his colleagues developed techniques to fill water-in-oil emulsions with an alginate gel derived from seaweed. “By a clever bit of chemistry, we can make an alginate gel in the aqueous phase, within a continuous oil phase, that gives you the body of a hard fat,” he says.
Speirs has had to adjust baking conditions to compensate for the higher moisture content of products containing the emulsion. However, he says that the mouthfeel of the bakery products is remarkably similar to versions containing higher amounts of saturated fat. “There is a lightening of the color, but certainly with the testing we’ve done, people don’t mind that,” he says.
Other food companies are turning to tropical oils such as palm oil to replace trans fats. Palm oil contains about 50% unsaturated and 50% saturated fats. According to Gerald McNeill, vice president of research and development at IOI Loders Croklaan, an edible oil supplier with US headquarters in Channahon, Illinois, palm oil is making a huge comeback after being decimated by anti-saturated-fat media campaigns in the 1970s. When McNeill first started working with palm oil, he thoroughly researched the literature on saturated fat. “If saturated fat was really that unhealthy and artery-clogging, I didn’t want to be involved with that,” he says. “I read all the literature, and I decided there was no evidence whatsoever that saturated fat has any effect on heart disease, good or bad.”
By heating palm oil to different temperatures and then cooling it and collecting the crystals that form, IOI Loders Croklaan has been able to separate palm oil into about a dozen fractions containing fatty acids with different properties, ranging from liquids to buttery textures to waxy solids. In addition, interesterification can be used to swap positions of fatty acids on the glycerol backbone, which confers additional functional properties to palm oil fractions.
McNeill and his coworkers can precisely match the physical properties of various partially hydrogenated oils used in baking and frying by blending the palm oil fractions in different proportions. “So far we’ve been able to match every partially hydrogenated vegetable oil that anybody has come to us to make a match for,” says McNeill.
Thus, many food manufacturers have come full circle, from saturated fat to trans fat to saturated fat again, albeit in a different form. “The solution for trans fat is saturated fat, which is laughable because trans fat was invented to replace saturated fat,” says McNeill.
Sidebar
Dietary fat and cancer
The evolution in scientific thinking about dietary fat and cancer has followed a similar narrative to that of dietary fat and heart disease.
The diet–cancer connection was a corollary to the diet–heart hypothesis pushed by Ancel Keys and others from the early 1950s forward. In fact, a report in 1982 by the National Research Council (NRC) suggested the evidence supporting the association of dietary fat with cancer was so irrefutable that the report likened those researchers who remained skeptical with “certain interested parties [who] formerly argued that the association between lung cancer and smoking was not causational.”
To date, the most extensive literature review on cancer prevention is the continuing evaluation undertaken by the World Cancer Research Fund International (WCRF; www.wcrf.org) and the American Institute for Cancer Research (AICR; www.aicr.org). The groups’ first report was published in 1997.
“At the time of the 1997 WCRF/AICR review, it was recognized that associations between dietary fat and risk of breast cancer seen in case-control studies had not been confirmed in prospective studies with substantial statistical power,” wrote a team of epidemiologists from the University of Oxford and Harvard University in Public Health Nutrition (https://dx.doi.org/10.1079/PHN2003588, 2004). “Similar differences in results have now been observed for fat intake in relation to incidence of colon and lung cancers.”
The most recent WCRF/AICR report on Food, Nutrition, Physical Activity, and the Prevention of Cancer: A Global Perspective appeared in 2007 and reflects the evolution in thinking. The groups commissioned nine systematic literature review teams, each with 22 panelists, to synthesize the literature on nutrition, physical activity, and cancer. The panelists studied 7,000 articles, reviews, and meta-analyses in all languages. Team findings went to an international panel that synthesized information for many different cancers to come up with the report’s main recommendations.
The panel found that there is “only limited evidence suggesting that diets relatively high in fats and oils (in total, or any type) are in themselves a cause of any cancer.” As the report notes, this finding runs counter to previous reports. Overall, the panel decided that the evidence on fats and oils did not justify any judgment that rose to a “convincing” or “probable” level to associate dietary fat with the risk of cancer. In particular, the panel said, “saturated fatty acids . . . have no special relevance to the risk of cancer” (p. 371 of the report; https://tinyurl.com/WCRF-AICR).
Related Resources
Lipid Library
Edible Oil Processing
In the present context, the term edible oil processing covers the range of industrial…
Lipid Library
The Highs and Lows of Cannabis Testing
October 2016 With increasing legalization of both adult recreational and medical cannabis,…
Lipid Library
The secrets of Belgian chocolate
By Laura Cassiday May 2012 Like a bonbon nestled snugly in a…