The trouble with studying omega-3s and the brain
By Rebecca Guenard
January 2020
- Omega-3 research on the heart has suggested that the fatty acids positively benefit the cardiovascular system by controlling blood clotting and building cellular membranes.
- Although researchers have established that omega-3s are crucial for neural and vision development during pregnancy and the first few years of life, they have not yet determined how or if omega-3s help with brain function as we age.
- Some researchers question whether the fatty acid can even cross the blood-brain barrier. There is currently no way to know, but a new imaging technique may reveal the answer.
The US-based pharmacy CVS was recently ordered to refund the purchase price (about $31.00) of a falsely advertised dietary supplement. The pharmacy claimed the plant-derived form of the omega-3 fatty acid, docosahexaenoic acid (DHA), was clinically proven to improve memory. The advocacy group Center for Science in the Public Interest argued that CVS based its claim on research that, on the contrary, did not indicate that omega-3s boost cognitive function.
Health organizations around the world strongly recommend eating food rich in omega-3, since research indicating a benefit to the cardiovascular system continues to strengthen.
However, it is less clear what the brain can garner from this group of fatty acids. Richard Bazinet, associate professor of nutritional science at the University of Toronto in Ontario, Canada, says that 30 years ago researchers noticed that infants who were breast fed had higher levels of docosahexaenoic acid (DHA) in the brain than infants who consumed formula. At the time, infant formula was not supplemented with the fatty acid. That observation sparked more research on the compound’s purpose in the brain and the nutritional choices that ensure a sufficient supply.
“Preclinically, this was easy,” Bazinet says. “Lowering brain DHA levels in animals shows that the molecule is very important in regulating a lot of brain functions. Nutritionally in humans, this gets really complicated.”
The 1994 study of infant brain tissue proved that DHA concentration could be altered by nutrition, presumably affecting a range of health issues. Over the past three decades, studies have sought to answer whether polyunsaturated fatty acids (PUFAs) in the diet can improve intelligence, reduce depression, minimize symptoms of schizophrenia, or slow the progression of Alzheimer’s disease. Through three decades of research, there have been mixed or slightly positive results on the brain benefits of omega-3s. After all this time, what have we learned about the function of fatty acid in the brain and the foods that help humans achieve a health benefit?
Function
The human brain is primarily composed of fat. Phospholipids account for almost half of the organ’s weight. One of the most important structural molecules is the fatty acid DHA, which comprises the cerebral cortex, synaptic membranes, mitochondria, retina photoreceptors, and more. Humans acquire omega-3s during development, but several factors determine the production of omega-3s throughout life.
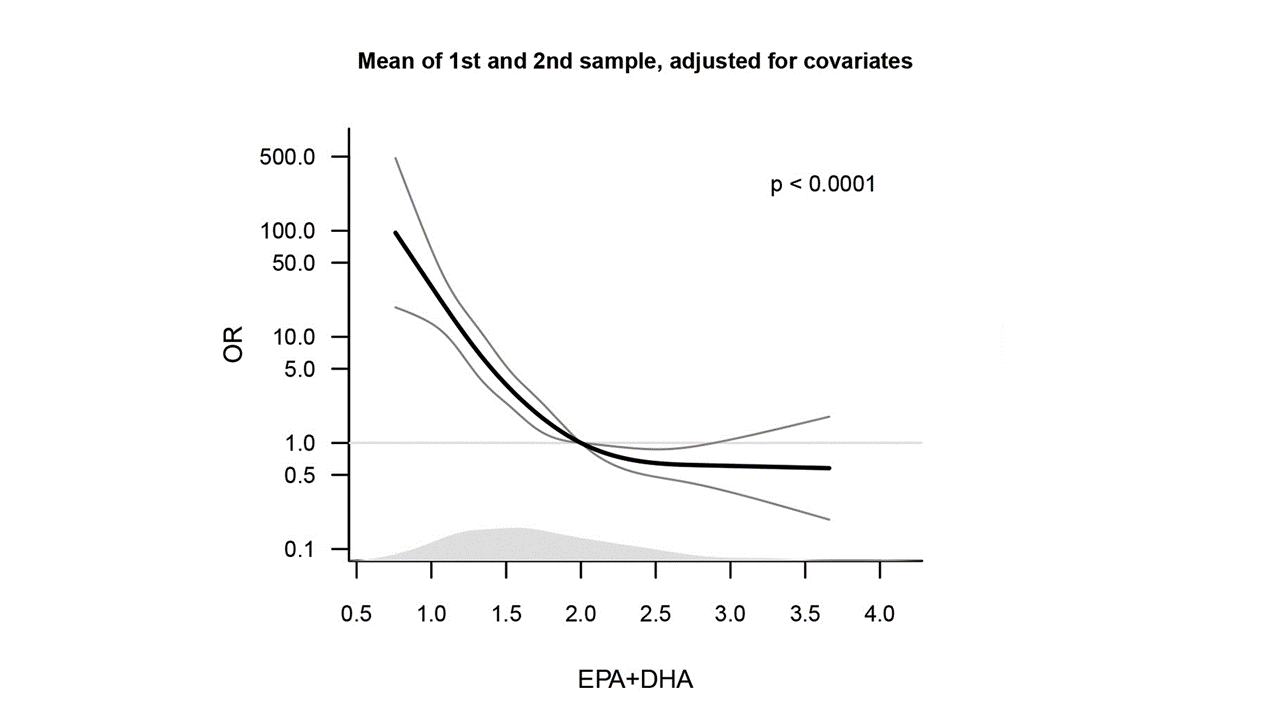
FIG. 1. A graph showing the importance of two types of maternal omega-3 concentration in blood plasma. The lower the concentration the lower the odds of the mother carrying the baby to term. Source: Olsen et al., EBioMedicine,35: 325, 2018.
For the first few years of life, humans are dependent on their mothers for essential fatty acids (Fig. 1). The fetus acquires DHA from maternal diet and the mother’s stored lipids. In the final trimester, maternal DHA levels drop dramatically as the fetus needs about half a gram a day to form its retina, liver, and brain. At birth, the human brain is about 70% developed and continues to grow for about six years. Infants obtain fatty acids from their diet. Human milk contains 30 times the DHA levels of milk from other animals. Since the 1990s, these crucial compounds have also been added to infant formula.
“We understand what the molecule does in the brain,” says Bazinet. “However, we do not understand very much about the regulation of brain levels in adults and how much nutrition you need to maintain those levels.”
Beyond the preschool years, humans have the metabolic capacity to synthesize specific omega-3s from the diet as needed, and no longer require a direct supply. Along with DHA, other nutritionally important omega-3 PUFAs, like eicosapentaenoic acid (EPA) and docosapentaenoic acid (DPA), are synthesized by an enzymatic desaturation of alpha-linolenic acid (ALA).
Though the mechanisms for formation are well-understood, they are less predictable inside the human body. For example, genetics can influence the speed and efficiency of these reactions. One study found that subjects with a desaturation gene variant convert ALA to important omega-3s more slowly than those without the variant, implying that supplementation may be effective at increasing omega-3 concentrations in the blood of some individuals, but not in others.
However, the amount of omega-3s in a person’s blood does not indicate the amount of omega-3s in the brain. To get an idea of how much of these molecules are in the brain, scientists rely on animals. Mouse studies show that omega-3 synthesis is rare in the brain and that levels are maintained by an accumulation in blood plasma from dietary sources. Both EPA and DHA appear to cross the blood-brain barrier in mice, but only DHA is detectable among the brain’s phospholipids.
“Despite not being detectable, new studies suggest that EPA gets in the brain and then gets metabolized very quickly,” Bazinet says. A recent study shows that EPA is metabolized into DHA and thus could be the key to reaping the benefits of this important omega-3. Some researchers believe EPA could alleviate a variety of brain-related ailments.
Mental health
Early studies on brain development and DHA revealed that maternal levels plummet at birth, which may be responsible for postpartum depression. Maternal plasma DHA levels drop by as much as 50% and may take up to six months to recover after delivery. Postpartum analysis of rats’ brains found that maternal brain DHA content after a single litter of pups can decrease by as much as 25% of its original level. The finding provoked further research into the role of DHA in mental health, revealing the importance of the compound for regulating dopamine.
The presence of PUFAs in brain membranes serve a variety of functions pertaining to neurological signaling. DHA is among a series of nuclear receptor ligands that participate in multiple transcription pathways involving dopamine. Neuronal and synaptic membranes contain high concentrations of DHA. The compound affects ion permeability, elasticity, protein function, phase behavior, and fusion. A range of studies confirm DHA’s involvement in the development and survival of dopamine systems within the brain.
Both animal and human studies indicate that omega-3 deficiencies during early brain development can alter dopamine upkeep in the organ leading to disorders like ADHD, depression, or schizophrenia (https://doi.org/10.2174/1871527317666180412153612). Researchers looked at specific tissue within the blood of schizophrenic patients and found that, compared to controls, they contain a lower amount of omega-3s. Low dietary and tissue levels of omega-3s in rodents have also consistently correlated with neurobiological indicators of depression. And some clinical trials involving symptomatic patients treated with omega-3 preparations have shown positive outcomes.
Antipsychotic drugs function by targeting dopamine receptors, and researchers theorize that some mental illness may result from an overactive dopamine system. By extension, omega-3s that assist in regulating dopamine are likely to help. Adult rats gestated and raised on omega-3-deficient diets showed a 70% reduction in brain DHA levels, and several areas of their dopamine system were defective. This has led many researchers to consider whether omega-3s should be incorporated in treatments for various mental health disorders.
However, in November 2019, a team of researchers at the University of East Anglia, United Kingdom, funded by the World Health Organization, published the results of a random-effects meta-analysis evaluating 31 clinical trials that assessed the effectiveness of long-chain omega-3 supplements in treating depression (https://doi.org/10.1192/bjp.2019.234). “Oily fish can be a very nutritious food as part of a balanced diet,” said Katherine Deane, the paper’s lead author. “But we found that there is no demonstrable value in people taking omega-3 oil supplements for the prevention or treatment of depression and anxiety.”
Despite all the evidence of DHA’s participation in crucial mechanisms of mental health, the finding on supplements indicates a gap in scientific understanding about how consuming omega-3 fatty acids can improve membrane concentrations established during development.
Cognition
The recent, successful lawsuit against CVS pharmacy highlights the many questions still swirling around omega-3s and the brain. Due to the participation of these molecules in the growth and repair of new neurons, researchers have assumed that omega-3 supplementation could prevent cognitive decline. The anti-inflammatory effect of fatty acids increase support for this hypothesis. Yet, as with other biological mechanisms involving omega-3s, there is little evidence showing cognitive improvement with supplementation.
New neurons are generated in the brain by different types of cells, but as we age this process, called neurogenesis, slows down. This slowing is accompanied by a decline in neuron maintenance. Animal studies have shown that EPA and DHA increase the growth of neurons in the developmental stage, but for aged rats, only DHA initiates improvements. These findings have inspired researchers to determine if neurogenesis and neuron survival could be improved in adult humans. However, many clinical studies have shown no difference between participants given treatment versus baseline scores for cognitive measures.
“I don't think anybody thinks omega-3s will increase your memory,” Bazinet says. “The idea is it will delay the decline in your memory with time.” He adds that quantifying such an effect is difficult to do since there will be no memory change in most adults during the duration of a clinical trial. “You have to look for people who are just starting to decline and test it in them,” he says. “It is a very hard thing to do.”
Here again, genetics complicates any study aimed at determining if omega-3s improve thinking and memory. Carriers of the ApoE-ɛ4 gene are more likely to develop late onset Alzheimer’s disease. This cohort also shows a lower response to EPA and DHA, and they are also less likely to experience improved cognitive function from eating fish. Scientists do not yet have a complete understanding of the gene and what it does, and more research is needed to fully understand its contribution to brain function with age.
One effect of aging that is better understood is the brain’s tendency toward inflammation. Studies of aged rats fed an EPA and DHA enriched diet concluded that the omega-3s had a clear anti-inflammatory effect. Another study performed on Alzheimer’s patients produced a similar result. Inflammatory markers like cytokines were significantly lower in patients who consumed a daily dose of EPA or DHA.
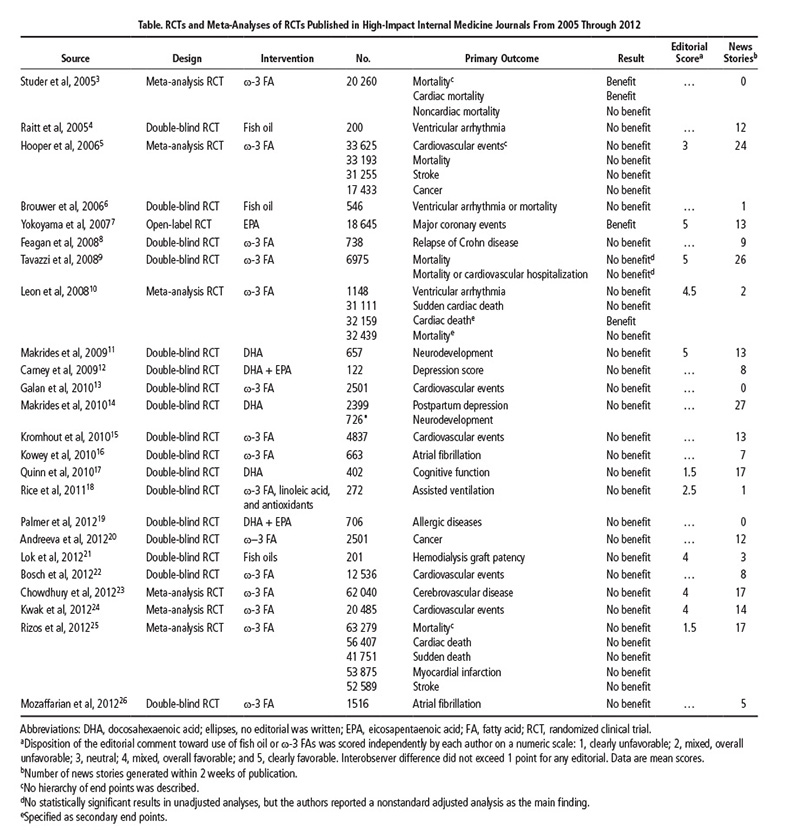
Still, deciphering the results of omega-3 studies can be tricky. As Bazinet mentioned, comparing preclinical studies on mice to clinical trials involving human plasma or tissue makes it challenging for researchers to draw overarching conclusions or dietary recommendations. Take fish studies, for example. It is unclear if simply eating fish improves health or if fish eaters have a higher socioeconomic status and cleaner lifestyle than non-fish eaters (Table 1).
“There are a lot of studies that look at groups of people that eat fish,” Bazinet says. “The results look good, but this is a correlation, cause and effect are hard to determine.” From a public health perspective, the cause is irrelevant, he says. If routinely eating fish reduces inflammation and improves cardiovascular health, then experts should encourage people to eat fish. As a scientist, Bazinet says he wants to understand more about why these benefits occur, so humans can maximize their potential.
Imaging
John Georgiadis is a biomedical engineer at Illinois Institute of Technology in Chicago, Illinois, USA. He has been using a new brain imaging technique that is growing in popularity and could help nutritionists like Bazinet study omega-3s in the living brain. In magnetic resonance elastography (MRE), a minor palpation of the brain during a typical scan reveals properties of the tissue that cannot be assessed otherwise. The resulting image is a map of tissue stiffness (https://doi.org/10.1016/j.neuroimage.2017.10.008).
Studies on healthy volunteers confirm that stiffness decreases with age. “You expect that with tangles and amyloid deposits the brain would be mostly hard material as we age,” says Georgiadis. The contrary is true, he says, because the deposits disrupt connections that maintain overall stiffness. “You can have hard regions in the brain tissue, but the rest is loose.”
Brain stiffness has been proven a strong indicator of cognitive performance and neurodegeneration. Studies show that stiffness decreases in diseases like multiple sclerosis and dementia. Additionally, the spatial pattern of stiffness and other viscoelastic properties indicate different brain ailments. Combined with other techniques, like diffusion tensor imaging (DTI), a highly sensitive type of magnetic resonance imaging (MRI) that maps water flow through white matter (https://doi.org/10.1016/j.nurt.2007.05.011), researchers can differentiate between brain changes at the microstructural and cellular level to evaluate if there is any effect from digested lipids.
Until now there have been few attempts to image DHA uptake in the living human brain because the procedure required complicated radiochemistry to acquire images. The only other option would be a brain biopsy which, not surprisingly, researchers are not willing to conduct on healthy humans. Studies on post-mortem samples comparing fatty acid content of plasma and brain tissue from the same individual suggests that plasma levels are not reflective of fatty acid concentrations in the brain. Imaging an ingested molecule as it travels the brain would be ideal.
“It is too simplistic to assume that just because the brain has more lipids than protein, we can affect its lipid content,” says Georgiadis. “The brain will do whatever it can to maintain function.”
So far, he has not performed MRE studies focusing on lipids as an aspect of the diet, but his group is currently in the process of submitting proposals to study specific nutrients and their effect on brain structure. As researchers improve the protocols for imaging techniques like MRE and DTI, they can apply them to more dietary studies. Though, as Bazinet points out, dietary double-blind trials are still a challenge. “Either you get the fish, or you get the hamburger.”
The brain stops accumulating DHA at around 18 months. Researchers believe that from conception to two years of age, the omega-3 fatty acid concentration can be increased by consumption; beyond that, they are not so sure. Their best assessment for omega-3 intake as we age is: It cannot hurt. Cardiovascular research indicates that omega-3s improve circulation, which means better blood flow to the brain and all the other organs. Consumers will have to be satisfied with that for now.
References
- Omega-3 and polyunsaturated fat for prevention of depression and anxiety symptoms: systematic review and meta-analysis of randomized trials, Deane, K., et al., Br. J. Psychiatry, 1–8, 2019.
- N-3 (omega-3) fatty acids: effects on brain dopamine systems and potential role in the etiology and treatment of neuropsychiatric disorders, Healy-Stoffel, M. and B. Levant, CNS Neurol. Disord. Drug Targets 17: 216–232, 2018.
- MR elastography of the brain and its application in neurological diseases, Murphy, M.C., et al., Neuroimage.187: 176–183, 2019.
- Long-chain omega-3 fatty acids and the brain: a review of the independent and shared effects of EPA, DPA, and DHA, Dyall, S.C., Front. Aging Neurosci.7: 52, 2015.
- Diffusion tensor imaging of the brain, Alexander, A.L., Neurotherapeutics 4: 316–329, 2007.