Omega-3 fatty acid profiling and dietary forensics
By Ken D. Stark
August 2009
Editor's note: The following article is based on the address given by Ken D. Stark, the 2009 AOCS Young Scientist Research Award winner, at the 100th AOCS Annual Meeting & Expo, held in Orlando, Florida, USA, May 3-6.
The quantity and type of dietary fat intake influence cellular membrane composition and lipid metabolism, which can impact cardiovascular disease (CVD), obesity, inflammation, and neurological development and function. Consumption of some types of fatty acids, such as omega-3 fatty acids, provides health benefits, while others, such as saturated and trans fatty acids, can potentially increase the risk of disease. Assessing individual dietary and cellular fatty acids, and determining their specific impact on biological processes, is becoming increasingly important. For example, whereas ª-linolenic acid (ALA, 18:3n-3), eicosapentaenoic acid (EPA, 20:5n-3), n-3 docosapentaenoic acid (DPAn-3, 22:5n-3), and docosahexaenoic acid (DHA, 22:6n-3) are all omega-3 fatty acids, they accumulate in different lipids and tissues, and we are continually defining their distinct roles in health and disease.
Nutrient intakes including fatty acids can be estimated at the population level through aggregate methods such as food disappearance data, but for clinical utility, approaches that provide data specific to individuals are required. Estimates of an individual's dietary intake can be completed by average intake methods that involve food frequency questionnaires and surveys, and by daily food consumption methods that include recent intake recall and food diaries. Assessing nutrient intakes at the level of the individual is associated with a series of limitations that are spread throughout the process of estimating the actual intake. This includes the skill and consistency of the researcher during participant interviews, and the participant's ability to accurately report his or her intake and the ability to resist tendencies to change dietary habits during the observation process. There is also potential for errors and inconsistencies in handling the reports, both at the level of the researcher and in the software being used. Finally, the dietary assessment is limited by the actual food database being utilized. This includes potential errors in the accuracy and precision of the existing data, inconsistent methodological approaches to generate nutrient composition data, the completeness of the data, and the constantly changing food supply.
Determinations of fatty acids in human tissues and blood are biomarkers of dietary intake, but predicting fat intakes is difficult and dependent on the type(s) of fatty acid being examined. Approximately 90% of dietary fatty acid intake in modernized countries (including Japan) is comprised of four fatty acids: 16:0, 18:0, 18:1n-9, and 18:2n-6 (palmitic, stearic, oleic, and linoleic acid, respectively). Endogenous fatty acid synthesis limits the utility of several biomarkers, especially saturated fatty acids. Fatty acid tissue-diet biomarkers with the most potential are those fatty acids exogenously obtained through the diet and include polyunsaturated fatty acids, trans fatty acids, and odd-numbered carbon-chain fatty acids. DHA in erythrocytes and plasma correlates highly with dietary DHA intake. Pentadecanoic (15:0) and heptadecanoic (17:0) fatty acids are associated primarily with dairy consumption, but they may help identify levels of saturated fat intake. Determining saturated fatty acid tissue biomarkers for the intake of individual dietary saturates is difficult, but the use of ratios and/or sums and aggregates of fatty acids can allow for the prediction of differences in polyunsaturated fat intake vs. saturated fat intake.
In addition, 16:1n-7 and 18:1n-7 are potential markers of low-fat/high-carbohydrate diets. Increased contents of n-7 fatty acids in tissues and blood reflect increased endogenous fatty acid production stimulated by excess carbohydrate intake. This increased endogenous 16:0 production results in increased ∆-9 desaturation of 16:0 (at the n-7 position) with potential elongation to 18:1n-7. Low exogenous fat intake reduces the availability of 18:1n-9 and 18:2n-6 and results in greater incorporation of n-7 fatty acids into tissue lipids. The use of models combining four to five fatty acids measured in blood have been successful in differentiating between moderate- and low-fat diets. Empirical relationships developed by Bill Lands for determining the fatty acid compositions of human plasma phospholipids from dietary intake are available online (http://efaeducation.nih.gov/sig/dietbalance.html ).
Blood-based biomarkers have a practical advantage over tissue-based biopsies. Adipose biopsies can provide very good, long-term dietary intake information, but they are far too invasive to be used at the level of routine clinical screening. Plasma and erythrocytes tend to be the blood fractions analyzed most often, although whole blood, platelets, and leukocytes have been analyzed as well. Plasma and erythrocyte measures tend to reflect shorter-term intakes, but they may be suitable for estimating long-term intake. The preparation of plasma-free erythrocytes and erythrocyte-lipid extraction requires specialized and time-consuming methodologies, but the fatty acid composition of the total lipid extract of erythrocytes is extremely similar to the fatty acid composition of erythrocyte phospholipids. Lipid class separation in erythrocytes prior to fatty acid determinations is unnecessary.
Plasma lipids, on the other hand, include triacylglycerols, cholesterol esters, and phospholipids. Fatty acid determinations of plasma total lipid extracts are often avoided because the fatty acids in the triacylglycerols component can be influenced by recent dietary intake and the triacyglyerol pool can be highly variable depending on whether the individual was in a fasted or fed state. Therefore, plasma-based fatty acid determinations are typically associated with prior lipid class separation such as thin-layer chromatography. A finger-tip-prick blood sample on chromatography paper is an extremely rapid blood collection technique that does not require trained phlebotomists and holds considerable potential for field studies and screening (Fig. 1). This technique does limit the results to the fatty acids composition of total lipids in whole blood, and it is very difficult to isolate specific blood fractions and individual lipid classes. However, it is important to point out that in the Physicians' Health Study, it was higher EPA + DHA levels in whole blood that was associated with lower risk of sudden cardiac death.

FIG. 1. Fingertip-prick blood sampling on chromatography paper.
The sum of the relative percentages of EPA and DHA in erythrocytes has been suggested as a potentially useful clinical risk factor, based largely on correlations to heart EPA + DHA status. An alternative method of examining omega-3 fatty acid status is to examine the percentage of omega-3 fatty acids in the highly unsaturated fatty acid pool (HUFA, ≥20 carbons and ≥3 double bonds). The HUFA pool is a surrogate marker of the fatty acids in the sn-2 position of cellular phospholipids. Focusing on the HUFA class of fatty acids allows estimation of cell membrane levels of omega-3 fatty acids from total lipid fatty acid determinations, without the necessity for blood fractionations and extensive isolation of lipid classes.
North Americans tend to have percentages of n-3 HUFA in total HUFA of about 20% in various blood measures, which is below the level of 50% that would provide significant cardio-protection. Using the percentage of n-3 HUFA in total HUFA also increases the ability to predict the omega-3 fatty acid status of tissues such as liver, brain, and heart from blood omega-3 fatty acid status. By using the percentage of n-3 HUFA in total HUFA, we are also able to employ a variety of high throughput processing techniques such as direct transesterification of fatty acids with microwave energy without sacrificing the accuracy of the estimate of omega-3 fatty acid status (Fig. 2).
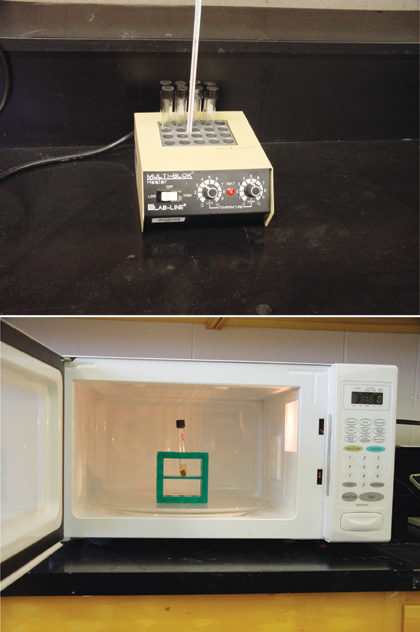
FIG. 2. Direct transesterification of fatty acids in blood lipids using boron trifluoride in methanol by traditional convectional heat (approximately 60 min) as compared with microwave energy (approximately 45 s).
Combining these processing techniques with fast gas chromatography can result in tremendous gains in sample throughput and increased cost efficiency, and a lower cost per sample. It is estimated that more than 350,000 North Americans die each year from sudden cardiac death, while fish oil supplementation is associated with a 45% reduction in the risk of sudden cardiac death. Regular monitoring of omega-3 fatty acid intakes through blood analyses could prove highly effective for first-line prevention of sudden cardiac death. High throughput, cost-efficient analytical methods could enable fatty acid determinations in large-scale clinical trails and potentially lead to routine clinical fatty acid profiling by health care professionals.
Ken Stark received an undergraduate degree from the University of Toronto and he completed his graduate studies at the University of Guelph. While at Guelph, he was an AOCS honored student. He spent two years at the National Institutes of Health as a post-doctoral fellow examining dietary and behavioral influences on maternal-fetal metabolism of fatty acids. He is currently an assistant professor in the Department of Kinesiology at the University of Waterloo where he heads the Laboratory of Nutritional & Nutraceutical Research. Contact him at kstark@uwaterloo.ca.
information
For further reading:
Albert, C.M., H. Campos, M.J. Stampfer, P.M. Ridker, J.E. Manson, W.C. Willett, and J. Ma, Blood levels of long-chain n-3 fatty acids and the risk of sudden death, N. Engl. J. Med. 346:1113-1118 (2002).
Armstrong, J.M., A.H. Metherel, and K.D. Stark, Direct microwave transesterification of fingertip prick blood samples for fatty acid determinations, Lipids 43:187-196 (2008).
Harris, W.S., and C. Von Schacky, The Omega-3 Index: A new risk factor for death from coronary heart disease? Prev. Med. 39:212-220 (2004).
Lands, W.E., Long-term fat intake and biomarkers, Am. J. Clin. Nutr. 61: 721S-725S (1995).
Stark, K.D., The percentage of n-3 highly unsaturated fatty acids in total HUFA as a biomarker for omega-3 fatty acid status in tissues, Lipids 43:45-53 (2008).
