Is it time to reconsider the role of saturated fats in the human diet? April 2022
By Rebecca Guenard
In This Section
- Microalgae’s impact on human and animal nutrition, April 2024
- Finding purpose and profit from waste, March 2024
- A low-cost, effective green extraction method, February 2024
- Establishing specialized nutrition in China, January 2024
- The disparity between protein sources and their nutritional value, November/December 2023
- Visualizing complex, multiphase food using confocal Raman microscopy, October 2023
- A more sustainable future begins with collaboration and data, September 2023
- Brain diets, July/August 2023
- Green coffee beans meet green tech, June 2023
- Fatty acid intake and inflammation, May 2023
- The Wild West of edible oils, April 2023
- The arc of preservation bends toward nature, March 2023
- Cloaking a cure: Lipid capsules save the world, February 2023
- From the farmers market to store shelves, January 2023
- Dogma vs. data: Rethinking linoleic acid, November/December 2022
- Improving food packaging, October 2022
- Proteins for meat alternatives: new competition for soy and wheat, September 2022
- Fish heads, fish heads: For biosurfactant production July/August 2022
- Mimicking mother’s milk June 2022
- Three paths forward for sustainable palm oil May 2022
- The continued struggle over biofuel feedstocks March 2022
- A new kind of plant breeding February 2022
- The new bio-based surfactant feedstock January 2022
- Lipid role in the immune system November/December 2021
- New essential dietary lipids? October 2021
- Gut Instincts September 2021
- Can computers make better plant-based foods? July/August 2021
- Poisson from a petri dish June 2021
- The latest additions to eco-friendly cleaning May 2021
- Preserving emulsions with plant-based antioxidants April 2021
- Developments in green surfactants for enhanced oil recovery March 2021
- Alternative base oils: a perspective March 2021
- The COVID-19 pandemic, one year later March 2021
- The green machine: commercializing microalgae products February 2021
- Bio-based (edible) oils: feedstock for lubricants of the future January 2021
- The latest on liposomes January 2021
- Fatty acids and athletic performance November/December 2020
- Where are lubricants headed November/December 2020
- New developments in vegetable oil materials science October 2020
- Agriculture at risk: preparing the oilseed industry for a warmer world September 2020
- Science highlights from a cancelled 2020 AM&E July/August 2020
- Managing your career in times of change June 2020
- Lipidomics comes of age May 2020
- Minimally processed oils April 2020
- The high-throughput frontier March 2020
- Nurturing innovation: how AOCS industries are fostering progress February 2020
- The trouble with studying omega-3s and the brain January 2020
- Understanding pulse anti-nutrients January 2020
- Digitizing manufacturing: how companies are using data to improve production November/December 2019
- Weaving together genetics, epigenetics, and the microbiome to optimize human nutrition October 2019
- Taking the cream out of ice cream September 2019
- Science highlights from St. Louis July/August 2019
- Biotechnology conquers consumer goods June 2019
- Cool characterization methods and where to find them May 2019
- Fermentation, the new protein supply chain April 2019
- Oleogels for drug delivery March 2019
- The complexity of clean-label cosmetics February 2019
- Rethinking plastic packaging January 2019
- Trends in synthetic and natural antioxidants for shelf life extension of meat and meat products November/December 2018
- The icing on the cake October 2018
- Enhancing oxidative stability and shelf life of frying oils with antioxidants September 2018
- Under arrest: investigating factors that govern partial coalescence July/August 2018
- Unconventional Oils June 2018
- Beauty from within May 2018
- Pulses rising April 2018
- Lessons learned from Hurricane Harvey March 2018
- Clean meat February 2018
- What makes your shortening suitable for fancy croissants, puff and Danish pastry? January 2018
- Strategic role of peanuts in sustainable global food security November/December 2017
- Science beyond borders: international student exchange October 2017
- Clean label: the next generation September 2017
- Science snapshots from Orlando July/August 2017
- Five new AOCS methods June 2017
- The whys and wherefores of life-cycle assessment May 2017
- China’s evolving edible oils industry April 2017
- The mysterious case of the arsenolipids March 2017
- Red palm oil February 2017
- The Highs and Lows of Cannabis Testing October 2016
- Chia: Superfood or superfad? January 2017
- Generational training divide November/December 2016
- Storage stability of roasted nuts and stabilization strategy using natural antioxidants September 2016
- Good vibrations: online and at-line monitoring of edible oils with vibrational spectroscopy July/August 2016
- Benchtop NMR spectroscopy for meat authentication June 2016
- Coconut oil boom May 2016
- Sink or swim: fish oil supplements and human health April 2016
- Pulsed electric field: groundbreaking technology for improving olive oil extraction March 2016
- Prescribing dietary fat: therapeutic uses of ketogenic diets February 2016
- Organogels of vegetable oil with plant wax January 2016
- The power of peptides November/December 2015
- Separation anxiety: membrane cleaning in the 21st century October 2015
- Using direct solid phase extraction to analyze persistent organic pollutants in oily food samples September 2015
- Big fat controversy: changing opinions about saturated fats June 2015
- Use of spent bleaching earth for economic and environmental benefit May 2015
- An introduction to cosmetic technology April 2015
- Food texture and nutrition: the changing roles of hydrocolloids and food fibers March 2015
- Scientists rank thousands of substances according to potential exposure level March 2015
- Clean smell does not always equal clean air February 2015
- Biotechnology: Using living systems to solve problems February 2015
- Flush to fuel January 2015
- 1970s fish oil study criticized January 2015
- Developing a high-performance, low-streak degreaser November/December 2014
- Detection, monitoring, and deleterious health effects of lipid oxidation November/December 2014
- Modified protein mimics taste and texture of fat October 2014
- Development of the first efficient membrane separations of cis fatty acids October 2014
- Regulatory updates on FSMA and combustible dust September 2014
- How enzymes are transforming manufacturing September 2014
- Two advances in biodiesel technology July/August 2014
- 2014 AOCS Annual Meeting & Expo July 2014
- Peanut genome sequenced June 2014
- A customized approach to frying oil June 2014
- Omics reveals subtle changes in carbon flux that lead to increased oil biosynthesis in oil palm May 2014
- Cannabis testing: a review of the current landscape May 2014
- Industrial hemp gaining traction April 2014
- Emulsions: making oil and water mix April 2014
- Lipid co-oxidation of proteins: One size does not fit all March 2014
- FSMA marches on March 2014
- Disruptive technology? Walmart’s “green” product line may signal a big change February 2014
- Pathways to novel chemicals February 2014
- Specialty lipids in pet nutrition January 2014
- EFSA releases preliminary report on occurrence of 3-MCPD in food January 2014
- Seven new biobased surfactant technologies November/December 2013
- Do oil color scales make you see red . . . or yellow? November/December 2013
- Shortage leads to green route to olefins October 2013
- Sesamol: a natural antioxidant for frying oil September 2013
- FSMA update September 2013
- Patent rights and biotech seeds July August 2013
- The other vitamin E July 2013
- Frac fever heats up June 2013
- Fat fight: Catch-22 for Western oleochemicals? June 2013
- Health and Nutrition News April 2013
- FDA asks for fees from industry to fund FSMA June 2013
- What does it take to start a biodiesel industry? April 2013
- What’s in a Claim? Would a Food Not Labeled “Natural” Taste as Sweet? March 2013
- Regulatory overview March 2013
- The preservative wars February 2013
- Plants producing DHA February 2013
- Swift response to paper on feeding GMO corn, glyphosate January 2013
- AOCS: supporting international standards January 2013
- TSCA and the regulation of renewable chemicals July August 2013
- trans Fatty acid content of foods in China January 2013
- A novel green catalytic process for biodiesel production from Jatropha November/December 2012
- The America Invents Act: Groundbreaking US patent law changes are here November/December 2012
- “Super Phos” esters: the key to higher-performance products November/December 2012
- Advances in field-portable mass spectrometers for on-site analytics October 2012
- EFSA sets upper intake level for LC-PUFA October 2012
- Malaysia: economic transformation advances oil palm industry September 2012
- High-oleic canola oils and their food applications September 2012
- Using enzymes to prepare biobased surfactants July/August 2012
- Oilseeds: at the center of food, water, and energy security July/August 2012
- Health & Nutrition News June 2012
- Hydrocolloids get personal June 2012
- The secrets of Belgian chocolate May 2012
- Plants “remember” drought, adapt May 2012
- The power of mass spectrometry in the detection of fraud April 2012
- Oil in biomass: a step-change for bioenergy production? April 2012
- The Future of LAB March 2012
- World supplies of rapeseed and canola likely to remain tight in the 2012/13 season March 2012
- Methods for differentiating recycled cooking oil needed in China February 2012
- Supercritical fluid-based extraction/processing: then and now February 2012
- Singapore: the place to be in 2012 February 2012
- The Food Safety Modernization Act and its relevance to the oilseed industry February 2012
- Oilseeds in Australia January 2012
- Hydrogen peroxide in home-care formulations November 2011
- A new generation of renewable fuels is on the horizon November 2011
- Omega-3 fatty acids: $13 billion global market October 2011
- Soy and breast cancer October 2011
- EU approves food labeling rules September 2011
- IOM panel recommends tripling vitamin D intake: Panel’s conservative approach receives criticism September 2011
- Self-assembly of lyotropic liquid crystals: from fundamentals to applications August 2011
- Sustainability watch July 2011
- Sustainability Watch July 2011
- Are algae really feasible as fuel? June 2011
- The trouble with crystal polymorphism June 2011
- Insect oils: Nutritional and industrial applications May 2011
- Reconstructing formulas April 2011
- US eggs now lower in cholesterol April 2011
- How to control eating behavior--in mice March 2011
- Maybe we don’t know beans March 2011
- Short- and long-term price forecasting for palm and lauric oils February 2011
- New 3-MCPD (glycidol ester) method February 2011
- Regulatory issues associated with the international oils & fats trade January 2011
- Point-counterpoint on UC Davis olive oil report January 2011
- Biomass--The next revolution in surfactants? December 2010
- One person’s response to a high omega-6 diet November 2010
- Crop residues as feedstock for renewable fuels November 2010
- Universal detectors for determination of lipids in biodiesel production October 2010
- New very long chain fatty acid seed oils produced through introduction of strategic genes into Brassica carinata October 2010
- Surfactants based on monounsaturated fatty acids for enhanced oil recovery September 2010
- Questioning the virginity of olive oils September 2010
- Dietary guidelines report released August 2010
- Keeping up with detergent chemistry August 2010
- News from the Expo floor July 2010
- Degumming revisited July 2010
- First high-GLA safflower oil on market June 2010
- AOCS 2.0 debuts June 2010
- Palm fatty acid distillate biodiesel: Next-generation palm biodiesel May 2010
- Palm oil pundit speaks May 2010
- What is unrefined, extra virgin cold-pressed avocado oil? April 2010
- The ultra-low-linolenic soybean market April 2010
- Dealing with the media: A cautionary tale March 2010
- Hempseed oil in a nutshell March 2010
- Carbon management 101: A conversation with Eric Jackson February 2010
- Giants of the Past: Hermann Pardun (1908-2009) February 2010
- Q&A with Bill Christie February 2010
- Update on Jatropha January 2010
- Unique properties of carbon dioxide-expanded lipids January 2010
- The market situation and political framework in Germany for biodiesel and vegetable oil December 2009
- Industrial oil crops-when will they finally deliver on their promise ? December 2009
- Chemically enhanced oil recovery stages a comeback November 2009
- Field-portable mass spectrometers for onsite analytics: What's next? October 2009
- To make biofuels, or not to make biofuels:That is the question. September 2009
- Melamine analysis at the forefront September 2009
- Global oil yields: Have we got it seriously wrong? August 2009
- Omega-3 fatty acid profiling and dietary forensics August 2009
- Oilseeds of the future part 3 July 2009
- The rise and fall of surfactants lore July 2009
- Oilseeds of the future: Part 2 June 2009
- Codex Alimentarius Commission update June 2009
- Raw material sources for the long-chain omega-3 market:Trends and sustainability. Part 3. May 2009
- Oilseeds of the future: Part 1 May 2009
- Chloroesters in foods: An emerging issue April 2009
- Raw material sources for the long-chain omega-3 market: Trends and sustainability. Part 2. April 2009
- Synthetic HDL created March 2009
- Raw material sources for the long-chain omega-3 market:Trends and sustainability. Part 1. March 2009
- A convenient way to increase legume intake February 2009
- Vitamin E’s safety controversy January 2009
- Universal mechanism of aging uncovered? January 2009
- Is it time to reconsider the role of saturated fats in the human diet? April 2022
April 2022
- Dietary guidelines from multiple sources recommend people limit the amount of saturated fats in their diets.
- Some researchers say there is not a clear enough picture of how fats function in the body to assume saturated fats play a nefarious role.
- Recent findings on in vivo fat behavior indicate we need more science on saturated fats.
According to the World Health Organization (WHO), “existing evidence suggests that the intake of fatty acids is a major determinant of the serum lipid and lipoprotein profile.” When measured through blood tests their values can determine a person’s risk for cardiovascular disease (CVD). Numerous epidemiological studies associate high amounts of total cholesterol and triglycerides with the disease. Moreover, studies have shown the effect is cumulative and large amounts of lipids in a young individual predict later incidence of CVD.
The extensive findings on the relationship between fatty acid intake and CVD supported the idea, particularly in the United States, that decreasing fat in the diet would result in a lean, healthy population. Public policy enforced this ideology for 40 years. In that time, rates of obesity and diabetes grew, prompting some scientists to question the basis for a low-fat diet.
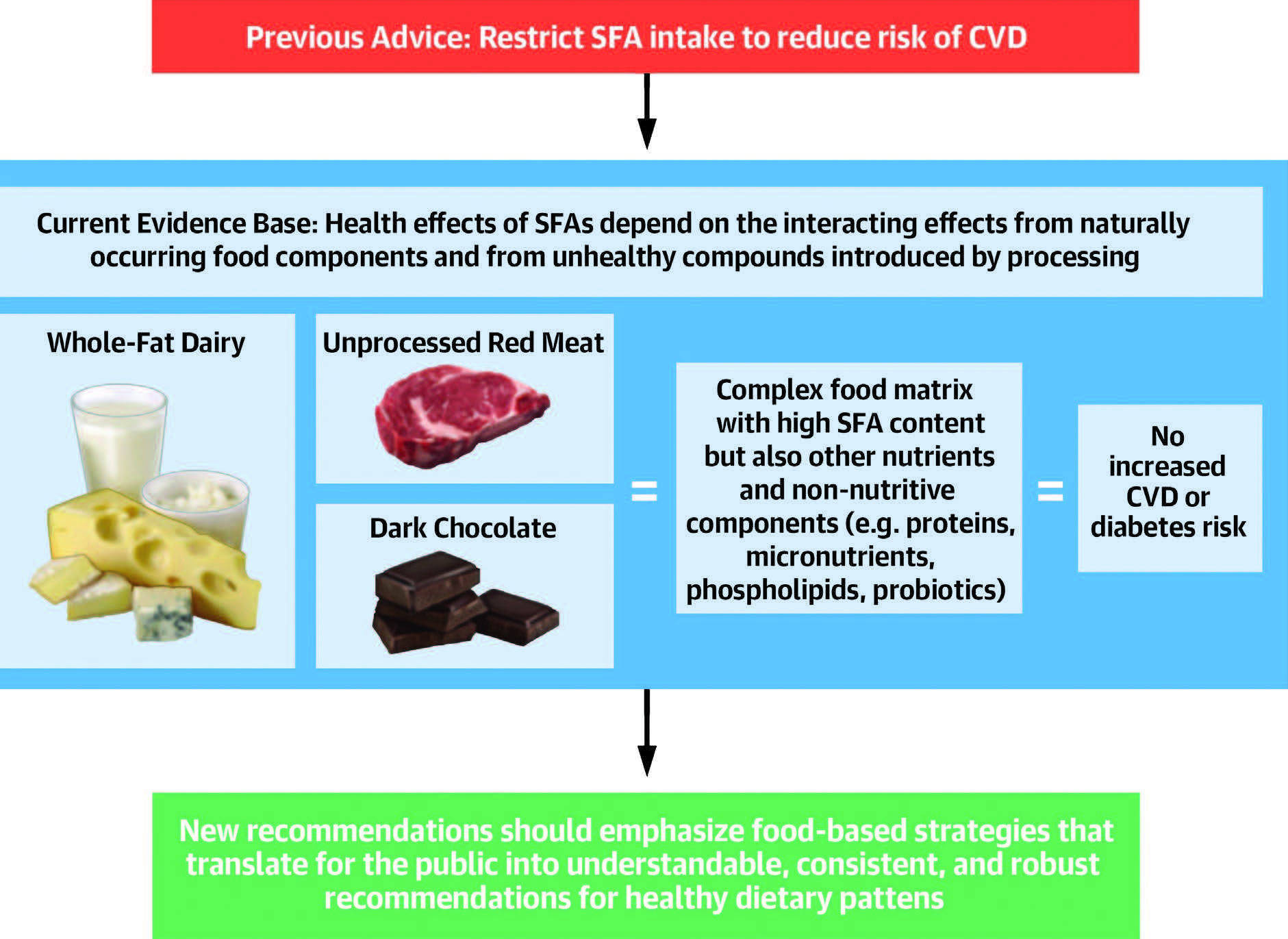
Scrutiny of dietary fat research over the last two decades has revealed the importance of discerning between types of fat. As a result, the majority of health agencies around the world have banned trans-fatty acids as an artificial food ingredient. (Calculations in the US indicate that trans-fat bans reduced CVD mortality by 4.5% (https://doi.org/10.1016/j.jhealeco.2015.09.005).)
Further analyses of research findings has also confirmed the health benefits of unsaturated fatty acids. The fate of saturated fats, however, still awaits consensus. Most guidelines recommend their consumption be limited, but some scientists question whether we have a clear enough understanding of the function of saturated fats in the body.
“I always circle back to the fact that the current dietary recommendations have been vetted,” says Penny Kris-Etherton, professor of nutritional sciences at The Pennsylvania State University in University Park, Pennsylvania, USA. “The Dietary Guidelines for Americans say there is strong evidence that saturated fats increase LDL cholesterol and that is a risk factor for CVD.”
Current Guidelines
For the unfamiliar reader, dietary fats consist mainly of triglycerides—a molecule with three fatty acids attached to a glycerol backbone. The properties of the molecule depend on its fatty acid composition. The number and location of their double bonds, as well as the length of their carbon chains distinguish fatty acids from each other.
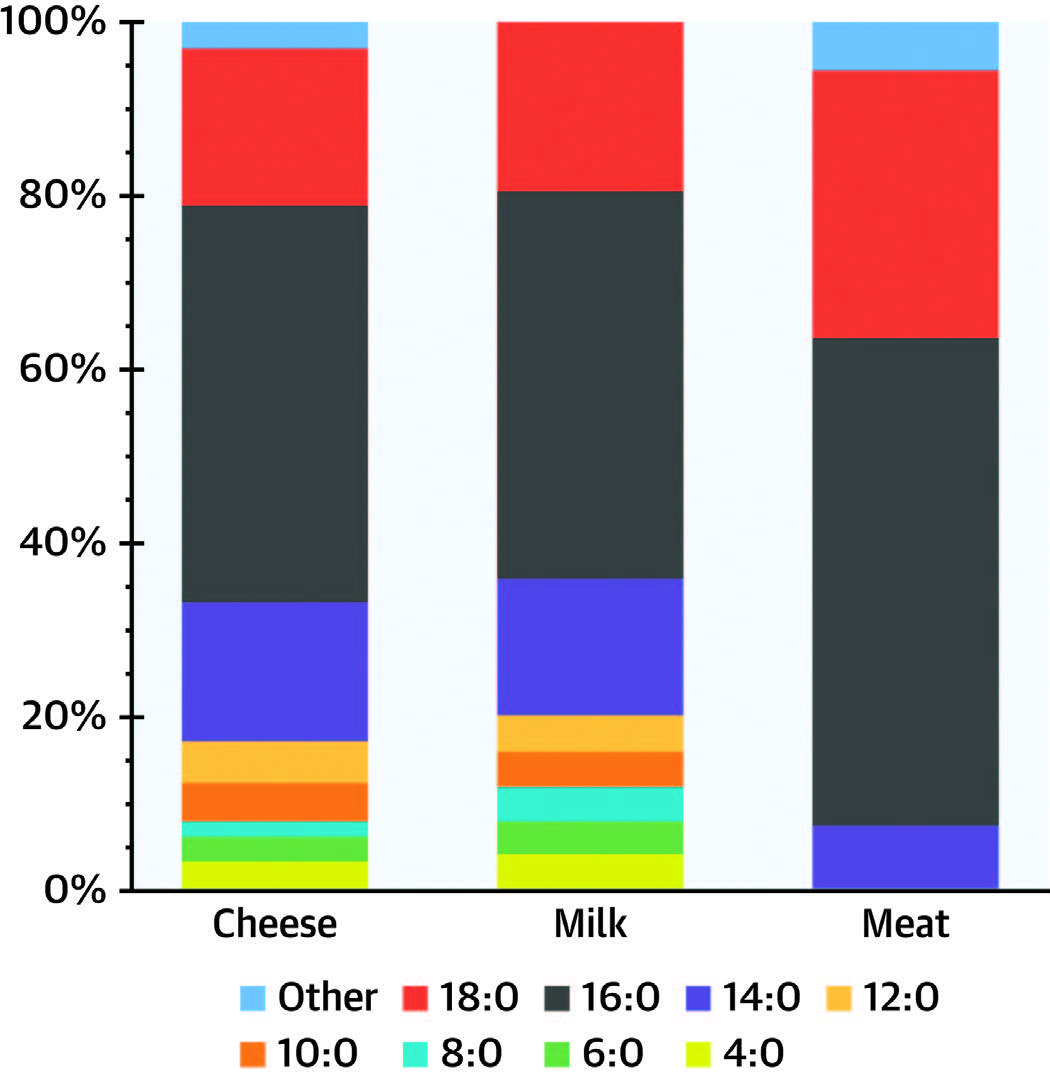
Saturated fatty acids (SFA) have no double bonds, while monounsaturated fatty acids (MUFA) have one double bond and polyunsaturated fatty acids (PUFA) have two or more double bonds. The WHO says the most abundant SFA in the diet have 16 (C16:0; palmitic acid) or 18 (C18:0; stearic acid) carbon atoms. Oleic acid (C18:1) is the most abundant MUFA and the most abundant PUFA are linoleic acid (C18:2n-6) and α-linolenic acid (C18:3n-3).
In 2016 Ronald Mensink, professor of molecular nutrition at Maastricht University, the Netherlands, conducted a systematic review of 84 dietary studies for the WHO to evaluate what happens to serum lipid and lipoprotein levels when MUFA, PUFA or carbohydrates replace SFA in the diet (https:// apps.who.int/iris/handle/10665/338049). The researchers assessed total cholesterol, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, triglyceride, LDL cholesterol to HDL cholesterol ratio, total cholesterol to HDL cholesterol ratio, triglyceride to HDL cholesterol ratio, apolipoprotein A-I (ApoA-I) and apolipoprotein B (ApoB).
Mensink performed a multiple regression analysis and found that subjects had a more favorable serum lipoprotein profile when they increased PUFA and MUFA in a diet that still contained SFA instead of replacing it with a mixture of carbohydrates. He specified that partially replacing SFA with PUFA had a greater effect on lowering LDL cholesterol and triglycerides. When SFA intake remained below 10% of a subject’s total energy intake, the individual maintained a desirable serum profile.
Based on Mensink’s study which corroborates with many others, the WHO now indicates that maintaining cardiovascular health means reducing SFA intake to less than 10% of calories. Current US guidelines also advise this threshold, while the American Heart Association recommends that people limit saturated fat consumption to 5-6% of their energy intake. That percentage is equivalent to about 13 grams a day for a 2,000 calorie diet. In the United Kingdom, the recommendation is no more than 20 grams per day for women, 30 grams for men.
SFA Distinctions
However, there are aspects of reviews on dietary fat research that leave some scientists wondering if saturated fats really contribute to chronic disease. When researchers dig into the data to determine the effect of individual SFA on serum profiles they find that there are differences. Cholesterol and triglyceride levels can go up or down for fatty acids like, lauric (C12:0), myristic (C14:0) or palmitic acid, while studies show stearic acid has no effect. This SFA specific variation of serum lipid profiles has prompted some to question if we have a complete understanding of how SFA behave in the body.
Kris-Etherton says that concentrating on types of SFA diverts attention from the more relevant point. “What some people would say is that there are some SFA that are better than others, but it is important to point out that individual saturated fatty acids are not as good as unsaturated fats,” she says. “Stearic acid may be neutral, but it is not as good as oleic acid and linoleic acid.” Nevertheless, Kris-Etherton acknowledges there are interesting data to suggest we need to start paying attention to the food matrix.
“There is wider evidence that foods have different properties because of the rich mix of nutrients, vitamins, minerals, and phytochemicals which together make up what is called the food matrix,” said Nita Forouhi, population health and nutrition professor at the University of Cambridge, School of Clinical Medicine, in Cambridge, England, UK, when interviewed by the online magazine verywellhealth (https://tinyurl.com/yckvkr2u).
The Company SFA Keep
Last November, Forouhi and a team of researchers evaluated data from the European Prospective Investigation into Cancer and Nutrition (EPIC) study. They compared the dietary habits of 10,529 people in 10 European countries who developed heart disease against 16,730 people who did not (https://doi. org/10.1161/JAHA.120.019814).
After accounting for other factors that might influence heart disease like, age, sex, and lifestyle choices, such as smoking, Forouhi and her team found that total dietary fat intake did not determine a person’s chance of developing heart disease. However, when they stratified the SFA by their food sources the team came to a different conclusion.
Nearly 80% of participants in the study consumed an excess of SFA, more than dietary guidelines recommend. Again, the high level of SFA alone did not represent a risk factor. Instead, they determined SFA from red meat and butter raised serum lipid levels in participants more than when they ate cheese, yoghurt, or fish. In their paper, Forouhi’s team points out that fermented dairy generates Vitamin K and bioactive peptides, in addition to the probiotics that exist, which could counter the negative effects of SFA.
Forouhi acknowledges that her studies are observational and prohibit the assignment of a cause and effect. Based on the results of previous studies; however, a growing body of research does support some of her findings. The isomer composition of an SFA seems to influence its in-vivo behavior, with odd-chain SFA affecting serum lipids differently than evenchain SFA. Eating palmitic acid, for example, has been shown to increase blood cholesterol levels while pentadecanoic acid (C15:0) consumption may lower the risk of heart disease (https://tinyurl.com/4r95by8x). The former is more often found in red meat, the later in dairy. (For more on odd-chain fatty acids see INFORM, Oct 2021, https://tinyurl.com/42weebmz)
One research team argues that conjuncture based on observed associations does not sufficiently explain the role of SFA. Marit Kolby (formerly Marit Kolby Zinöcker), assistant professor of nutrition at Oslo New University College, in Oslo, Norway has proposed that studying short-term changes in serum lipid profiles does not provide an adequate understanding of dietary fats in the body throughout a lifetime.
A New Hypothesis
Like many researchers, Kolby is eager for direct evidence of a molecular mechanism that explains cholesterol’s role in developing CVD. In a paper published in The American Journal of Clinical Nutrition last year, she argues that no current models explain the response of serum lipoprotein levels when altering dietary fatty acids (https://doi.org/10.1093/ajcn/nqaa322). Instead of being a pathogenic process, Kolby’s team proposes serum changes could be part of cellular regulation of cholesterol in order to maintain homeostasis.
Kolby wanted an explanation for the association between SFA consumption and observed increases of LDL cholesterol in blood. “To me it was logical to start by looking at cells and membranes, because most of the body’s cholesterol is contained in membranes not in the blood,” she says. “I started looking for evidence that changes in intake of dietary fatty acids would affect regulatory mechanisms for cholesterol content in cell membranes.”
According to Kolby’s hypothesis, eating PUFA results in cell membranes that are fluid and require cholesterol from the blood to introduce stiffness into the membrane. Whereas, eating saturated fats leads to membranes that require less stabilization by cholesterol which instead flows into the blood stream. She presumes cholesterol in the bloodstream could be acting as a reserve to fortify cell membranes as needed (https://tinyurl.com/47sbjdxe).
“It is possible that inflammation—in concert with other metabolic abnormalities, like insulin resistance—causes an increase in blood cholesterol due to dysfunctional lipid uptake and/or metabolism,” says Kolby. This would provide an alternative explanation for why high cholesterol leads to heart disease. Eating whole foods instead of ultra-processed foods, moving enough, sleeping enough, stressing less, and keeping good social relations to avoid chronic inflammation is more important than avoiding saturated fat, she says.
Time, and more research, will tell if Kolby’s hypothesis has clout, but findings in other areas of lipids research indicate we may be misunderstanding how the body uses fat stores.
Emerging Ideas
There is other evidence that stockpiles of lipids do not necessarily mean a sign of disease. In the September 2021 issue of INFORM magazine, we reported on a research group led by Alex Gould at The Francis Crick Institute in London, UK, using the Drosophila fruit fly to study lipid droplets (https://tinyurl. com/ybndrbc8). Once considered pathogenic themselves, the tarnished reputation of lipid droplets may soon shine.
“The fact that they correlate with a disease does not mean they are causing that disease. Our work suggest that lipid droplets are actually one of the body’s ways of fighting back against the disease,” Gould told INFORM last year.
Lipid droplets were initially determined to serve as mere energy reserves, inertly waiting to provide a cell with fuel. But Gould discovered that they also perform an important role of protecting PUFAs during oxidative stress (https://doi.org/10.1016/j.cell.2015.09.020). He found that the droplets encapsulated dietary linoleic acid, for example, to prevent free radical formation and preserve vital PUFAs during cell development.
More recently, the researchers focused on surface proteins on lipid droplets within renal cells to understand their involvement in kidney disease. When they turned the genes that generate the enzymes that synthesize or digest triglycerides on and off, the team observed an effect on the fly’s cell health. The group ultimately concluded that when fruit flies feed on a high-fat diet, the renal cells protect the kidneys from damage by sequestering lipids into droplets (https://doi. org/10.1371/journal.pbio.30012302021).
In January, a different research group observed another unique service role that lipid droplets provide. Animal science professor Shihuan Kuang and his postdoc Feng Yue at Purdue University in Lafayette, IN, USA discovered that fat inside adult muscle stem cells determine how the stem cells behave (https://tinyurl.com/5tzrefkr).
When adult muscle cells are injured, latent stem cells become active to repair the injury. Lipid droplets accompany the stem cells when they arrive at the injury site. The researchers determined the cells could differentiate into two types of cells: muscle cells that repaired damage and selfrenewal cells to resupply the used stock. Kuang says the lipid droplets somehow maintain a healthy balance of cells. When there are more droplets around, the stem cells continue to divide. To keep the stem cells from dividing uncontrollably, as happens with cancer, the cells seem to deplete themselves of the droplets and return to a dormant state (https://tinyurl. com/bdzcehx3).
As new research on the good deeds conducted by lipid droplets continue to unfold, we have to remind ourselves not to draw any connections to human dietary choices. The experiments have only been conducted on cells and animals, thus far. However, these studies reveal that fat plays a more complex role in cellular function than we realize.
“For the scientists who say: ‘There are problems with the evidence.’ We should get more science and resolve some of the controversies,” says Kris-Etherton. “I tell people, pay attention to authoritative recommendations right now. That is the best thing we can do.”
About the Author
Rebecca Guenard is the associate editor of Inform at AOCS. She can be contacted at rebecca.guenard@aocs.org
Is it time to reconsider the role of saturated fats in the human diet? (.pdf)


